The COVID-19 pandemic is a landmark event in modern history, profoundly altering our way of life. Since its emergence in late 2019, COVID-19 has killed millions of people, collapsed economies, and pushed healthcare systems to their breaking point. The virus led to lockdowns, social distancing mandates, and the redefinition of daily routines. Fast forward to 2024, and we find ourselves asking a critical question: Is COVID gone?
The answer to this question isn’t straightforward. It requires examining not just where the virus stands today but also its trajectory, the role of vaccines, the mutations of the virus, global inequalities in healthcare, and the long-term societal and health impacts of the pandemic. In this article, we will comprehensively explore these aspects to understand whether COVID-19 is truly behind us or if it remains an ongoing concern.
The Origins of COVID-19
Before delving into whether COVID is gone, it’s essential to reflect on how it began. COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, was first identified in December 2019 in Wuhan, China. This virus is part of the broader coronavirus family, which includes other severe illnesses like SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome), as well as more common strains that cause mild illnesses like the common cold.
The virus spreads primarily through respiratory droplets produced when an infected person coughs, sneezes, or talks, and it can remain airborne in closed environments. Early on, scientists were perplexed by the virus’s high transmission rates, partly because asymptomatic individuals could unknowingly spread it. This led to its rapid spread across the globe.
COVID-19’s symptoms vary widely, ranging from mild, flu-like symptoms to severe pneumonia and organ failure. The elderly and those with underlying health conditions are particularly vulnerable. However, even young and otherwise healthy individuals have been hospitalized or have died from complications. In the first few months of the pandemic, it was clear that COVID-19 was far more dangerous than initially thought.
The Global Response and Impact
As the virus spread, governments worldwide took unprecedented measures to try to contain it. The early months of 2020 saw national lockdowns, border closures, quarantines, and stringent social distancing regulations. Schools, businesses, and entire cities were shut down, and countries struggled to balance protecting public health with preventing economic collapse.
1. Healthcare Systems in Crisis
Healthcare systems, even in developed countries, were pushed to the brink. Intensive care units (ICUs) were overwhelmed with critically ill patients, leading to shortages of ventilators, personal protective equipment (PPE), and even basic hospital supplies. Medical staff worked long, grueling shifts and were frequently exposed to the virus. Tragically, many healthcare professionals lost their lives, and numerous others faced significant burnout.
In countries with fragile healthcare infrastructures, the situation was even more dire. Hospitals overflowed with patients, and many were forced to set up makeshift medical centers in arenas or tents. Without adequate resources, many people died from lack of treatment.
2. Economic Fallout
The economic impact of COVID-19 was staggering. Global supply chains were severely disrupted, businesses—particularly in tourism, hospitality, and retail—faced closures, and unemployment soared. By mid-2020, the International Monetary Fund (IMF) reported that the global economy had contracted by over 3%, with some sectors seeing losses reminiscent of the Great Depression.
Governments around the world initiated large-scale economic stimulus programs to mitigate the damage, but the fallout was widespread. Many small and medium-sized businesses were unable to survive the lockdowns and restrictions. Workers, particularly in low-wage jobs or the gig economy, found themselves without financial security, amplifying existing inequalities.
3. Mental and Social Health Crisis
In addition to the economic and physical toll, COVID-19 left a deep psychological impact on society. Extended isolation from friends, family, and loved ones led to an increase in mental health issues, including anxiety, depression, and substance abuse. The concept of “social distancing” left many feeling emotionally distanced as well. For children and adolescents, the absence of in-person schooling, social activities, and routine caused developmental delays and academic setbacks.
Even though digital communication tools helped bridge some gaps, the absence of human interaction had lasting social and psychological consequences. COVID-19 also magnified existing social inequalities, with marginalized communities, essential workers, and low-income groups suffering disproportionately due to poor access to healthcare, protective measures, and economic support.
The Turning Point: Vaccines and Treatments
One of the most significant turning points in the battle against COVID-19 was the development of vaccines. In record time, scientists and pharmaceutical companies developed several highly effective vaccines. The Pfizer-BioNTech and Moderna vaccines, based on messenger RNA (mRNA) technology, were the first to receive emergency use authorization in late 2020. AstraZeneca, Johnson & Johnson, and other vaccines soon followed.
Vaccines played an essential role in reducing the severity of COVID-19, preventing hospitalizations, and significantly reducing death rates. Mass vaccination campaigns around the world provided a ray of hope in what had been a dark period. As of 2024, billions of people have been vaccinated, and many have received booster doses to combat waning immunity.
In parallel, antiviral treatments like remdesivir and monoclonal antibody therapies provided additional weapons in the fight against the virus, particularly for high-risk patients.
Is COVID Gone?
Despite the successes of vaccines and treatments, the question remains: Is COVID gone? While the situation is vastly improved compared to the height of the pandemic, COVID-19 has not been eradicated. Rather, it has shifted into what experts call an endemic phase—meaning the virus is still present but circulating at lower levels, much like the seasonal flu.
1. Endemicity: Living with COVID
Eradicating COVID-19 completely is an unlikely prospect. Historically, only one disease, smallpox, has been entirely eradicated through vaccines. For most other infectious diseases, even those with effective vaccines, complete elimination has been impossible.
COVID-19, like other respiratory viruses, is expected to become endemic, meaning it will continue to exist but cause far fewer severe cases due to widespread immunity—either from vaccination or prior infection. Much like influenza, it may result in seasonal surges, but with fewer cases resulting in hospitalization or death. The virus will still mutate, and new variants could emerge, but with vaccines and treatments, its overall impact should be reduced.
2. Variants and Vaccine Efficacy
One of the reasons COVID-19 has not disappeared is the virus’s ability to mutate. The Alpha, Beta, Delta, and Omicron variants were all more transmissible than the original strain, and some were partially resistant to the initial vaccines. While vaccines were modified to better address variants, new mutations remain a persistent challenge.
In response, pharmaceutical companies have developed booster shots to enhance immunity and target specific variants. Researchers are also working on universal vaccines that would provide broader protection against coronaviruses, reducing the need for frequent boosters.
For now, however, the continuous emergence of new variants suggests that COVID-19 will remain with us, though its severity and transmissibility may vary from year to year.
3. Vaccine Hesitancy and Global Inequities
A key reason why COVID-19 hasn’t been entirely controlled is the uneven distribution of vaccines and vaccine hesitancy. While wealthier nations have vaccinated large portions of their populations, many lower-income countries still struggle with access to vaccines and medical infrastructure. As of 2024, there are still regions with low vaccination rates, increasing the likelihood of continued outbreaks.
Moreover, vaccine hesitancy fueled by misinformation remains a significant problem, particularly in some parts of the world. Without higher global vaccination rates, the virus will continue to circulate, mutate, and pose a threat.
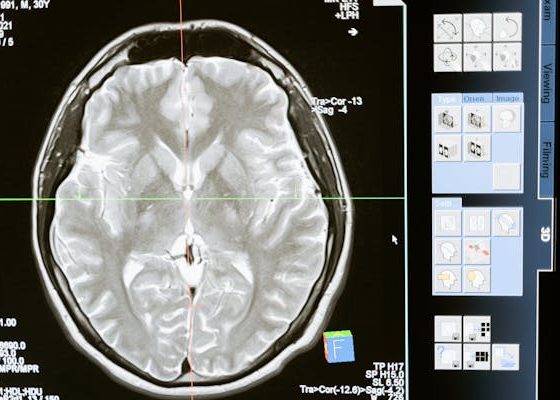
4. Long COVID: The Lingering Health Crisis
Even as COVID-19 becomes less deadly, the issue of Long COVID looms large. Many people who recover from COVID-19 experience lingering symptoms, such as fatigue, difficulty concentrating, shortness of breath, and joint pain. For some, these symptoms can last for months or even years after their initial infection.
Long COVID represents a significant public health concern. It is estimated that millions of people worldwide may be suffering from these long-term effects, placing an additional burden on healthcare systems. Governments and healthcare providers are still grappling with how to provide adequate support and treatment for Long COVID patients, which may persist as a challenge even if the acute phase of the pandemic fades.
The Global Status of COVID-19 in 2024
Today, the status of COVID-19 varies greatly by region. Many countries have managed to reduce transmission rates and return to normalcy, with mask mandates, travel restrictions, and lockdowns becoming things of the past. In countries with high vaccination rates, COVID-19 has largely become a manageable disease.
However, other regions continue to struggle. Low-income countries with poor access to vaccines and healthcare infrastructure still experience sporadic outbreaks. In some areas, misinformation and distrust of vaccines have led to lower immunization rates, prolonging the pandemic’s impact.
Furthermore, the emergence of variants could lead to localized spikes in cases, particularly in areas with low immunity. COVID-19 is unlikely to disappear entirely, but rather become a disease that requires ongoing management.
The Future: What Can We Expect?
Looking ahead, the future of COVID-19 will likely involve periodic vaccination campaigns, much like those for the flu. Some scientists are exploring the possibility of developing universal coronavirus vaccines, which would protect against multiple strains of the virus.
Researchers are also focusing on antiviral treatments that could prevent severe illness from COVID-19, particularly in high-risk populations. These advancements will be key in managing COVID-19 as an endemic disease.
The pandemic has also led to a renewed focus on global health infrastructure. Governments, international organizations, and healthcare institutions are now working to strengthen pandemic preparedness, ensuring that the world is better equipped to deal with future infectious disease outbreaks.
Conclusion:
The short answer to the question Is COVID gone? is no. COVID-19 has not been eradicated, and it is unlikely to disappear entirely. However, thanks to widespread vaccination, improved treatments, and public health measures, the world has moved beyond the most devastating phases of the pandemic.
COVID-19 will likely become an endemic virus, much like the seasonal flu. While it will continue to pose challenges, especially in under-vaccinated areas or where new variants emerge, it is no longer the global threat it once was. Instead, it is something we will manage through continued medical advancements, vaccinations, and public health efforts.
The journey through the pandemic has taught us many valuable lessons about preparedness, global cooperation, and the power of science. While COVID-19 may not be fully gone, our collective ability to overcome it and adapt gives us hope for a future where we are better equipped to handle similar challenges.